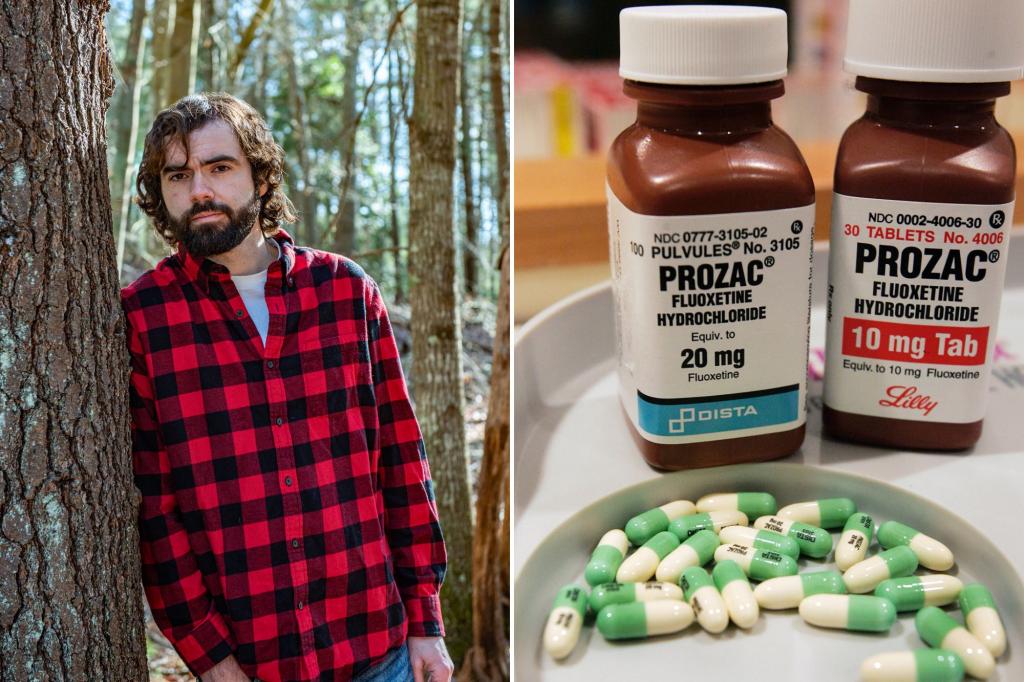
Nick Alves was 19 when a psychiatrist offered him the antidepressant Trintellix to treat his moderate anxiety and depression after just a few short visits.
Going on the popular selective serotonin reuptake inhibitor (SSRI) — a class of drugs that also includes Prozac — didn’t seem like a big deal at the time. But, when Alves went off the medication after six years, he immediately noticed his genitals were losing sensation.
Over the course of a couple weeks, he almost entirely lost feeling in the area — and it never returned, nor did the high sex drive he once had.
“That region feels as sensitive as the skin on the back of my elbow does,” said Alves, now 27 and a commercial truck driver in Massachusetts.
He would ultimately learn he suffers from Post-SSRI Sexual Dysfunction (PSSD).
For many, antidepressants are lifesaving treatments, but, in rare instances, they can potentially cause debilitating side effects that persist for years after stopping the drugs.
The medical establishment is increasingly recognizing these SSRI dangers, especially to young people, who are being prescribed them at a growing rate.
SNOMED, the National Institute Of Health’s official source of medical terminology for US healthcare systems, recognizes PSSD as a legitimate disorder as of this year, defining it as “persistent sexual side effects” including genital numbness and loss of libido that “can last for weeks, months, or even years after stopping” antidepressants.
The condition has also been acknowledged by official medical bodies in the United Kingdom and Australia, as well as the European Medicines Agency.
Warning labels for common antidepressants such as Prozac, Zoloft, and Paxil all list post-discontinuation sexual dysfunction as possible side effects.
“People feel pretty awful … and there isn’t anyone trying to find an answer to the problem,” David Healy, a psychopharmacologist and professor of psychiatry at McMaster University in Ontario, Canada, told The Post.
Alves can’t help but wish he’d been counseled differently in his teens and not been put on medication so hastily.
“I wasn’t at risk of taking my own life or anything like that … I still had a hell of a lot of fun in life … I think I definitely should have [done] therapy first and foremost,” he said. “Now there’s just no enjoyment in anything, like hobbies, or hanging out with my girlfriend, or watching a movie, or playing video games, my favorite thing to do, it’s all exactly the same. It’s like watching a brick wall.”
Research on PSSD has thus far been limited but concerning.
A 2023 study from researchers at Howard University and Tel-Aviv University published in the Annals of General Psychiatry retrospectively analyzed men seeking treatment for erectile dysfunction (ED), comparing subjects who had and hadn’t been on SSRIs previously.
Even when controlling for age and comorbidities, the research found that being on SSRIs was associated with a “significant” increased risk of erectile dysfunction. The researchers estimated the chances of developing PSSD among men who used antidepressants was 1 in 216.
The numbers are particularly staggering given the growing number of teens and young adults being prescribed antidepressants. According to the American Academy of Pediatrics, the rate of prescriptions for those ages 12 to 25 jumped by about two-thirds from 2016 to 2022, due in part to the pandemic.
Newly appointed Health and Human Services secretary Robert F. Kennedy Jr. has pledged to look into antidepressant side effects and possible overprescription to youth in his first meeting with staff.
Phillip, a 19-year-old from Maine who asked to withhold his last name for privacy reasons, said he was just six-years-old when he started what he calls a prescription medication “doom loop.”
That’s when his kindergarten teacher flagged him as having Attention-Deficit/Hyperactivity Disorder (ADHD) and a doctor prescribed Vyvanse, a stimulant often used to treat the disorder.
When he stopped taking the drug at age 12, he became depressed — a common temporary side effect of withdrawal from Vyvanse — so a doctor prescribed him Prozac.
Almost immediately, Phillip experienced sexual numbness and muted emotions. It’s been two years since he went off Prozac, but he feels the same.
“All the positive emotions are almost completely gone. I don’t feel the highs any more, but I felt all of them before the pills,” he thinks.
His doctors and therapists all agree with his PSSD diagnosis, though they’ve not been able to offer him any relief from his symptoms.
“I think it just messed with my developing brain,” he said. “Since I was going through puberty, it changed my blueprint … I feel like my body doesn’t have anything to revert back to.”
Elliott Blaise, a 24-year-old dishwasher from Atlanta, Georgia, was diagnosed with ADHD as a child and struggled with emotional outbursts, a common symptom of the developmental disorder.
When he was 18, a child psychiatrist prescribed him Zoloft to aid with emotional regulation.
The medication “didn’t help at all,” so he stopped after six months. Immediately, he noticed the typical PSSD symptoms of genital numbness and lack of emotion.
“No one can really comprehend what it’s like. You lose all spark in life, all enjoyment of things, everything just becomes bland and gray,” Blaise said. “It almost feels like I’m dead inside.”
Adding insult to injury is the fact that he has since been diagnosed as autistic and now believes he doesn’t actually have ADHD.
“I never had depression,” he told The Post. “They pretty much gave me the Zoloft for my autism.”
PSSD isn’t just impacting boys and young men.
Rebekah Kane was prescribed Zoloft at age 15 for Obsessive Compulsive Disorder (OCD), after her pediatrician referred her to a psychiatrist.
“There was no therapy or anything like that. It was just immediately medication,” Kane, now 24, told The Post.
Immediately, she experienced “complete” genital numbness as well as emotional numbness, but she brushed it aside.
“I wasn’t so worried about it, because in my mind it was a temporary trade off to get rid of the OCD at that moment,” she said.
After a year and a half on the medication, Kane, then 17, stopped Zoloft and headed to college to study pharmacology.
Her side effects never went away. They worsened with withdrawal. She tried other antidepressants to no avail.
“It feels like I was lobotomized, like the complete atmosphere of the world has gone,” she said. “The OCD was bad, but it was better than completely losing your identity as a person.”
Over-prescription among young people, despite potential serious side effects, is a growing concerning for Meg Jay, a clinical psychologist and University of Virginia professor of human development.
“There’s definitely a problem,” said Jay, who specializes in patients in their 20s. “Physicians are too quick to medicalize normal young adult struggles … In 15 minutes, they don’t get to hear much about the context.”
Over the course of her 25-year career, she’s noticed her patients being prescribed antidepressants at younger and younger ages — something that worries her, given the lack of research on how they impact developing brains.
“The studies that were done for SSRIs to be approved by the FDA were not done on children, they were done on adults,” she said. “But now it’s much more common for tweens and teens to be prescribed medications than it used to be.”
Heally agrees.
In the past two years alone, he said he’s known more than a dozen people, many of them young, who were so distressed by PSSD that they committed suicide.
“These teenage antidepressants are doing more harm than good,” he said. “Young people don’t typically get depressed, they get distressed … When you’re a teenager you go half crazy. Most of us do. It’s part of being a teenager, and you’ve got to learn to work it out and cope with the world.”
If you are struggling with suicidal thoughts or are experiencing a mental health crisis, you can call the 24/7 National Suicide Prevention hotline at 1-800-273-8255 or go to SuicidePreventionLifeline.org.
Read the full article here